A urethral stricture occurs when scar tissue forms within the urethra, causing it to narrow and restrict the flow of urine. This condition can lead to significant discomfort, recurrent urinary tract infections (UTIs), and, in severe cases, urinary retention, which requires immediate medical intervention. Urethral stricture surgery is the most effective treatment for correcting this narrowing and restoring normal urinary function.
Strictures of the urethra can occur at any age and are more common in men than in women due to anatomical differences. The narrowing can vary in length and location, making the condition unique to each patient. While mild cases may be managed with non-surgical methods, such as dilation or catheterization, severe or recurrent strictures often require urethral stricture surgery to prevent long-term complications.
Causes of Urethral Stricture
- Trauma: Injuries to the pelvic region or blunt trauma can cause scar tissue to form, leading to a urethral stricture.
- Infections: Infections, particularly sexually transmitted infections (STIs) like gonorrhea or chlamydia, can cause inflammation and scarring in the urethra.
- Medical Procedures: Surgical procedures involving the urethra, such as catheterization or prostate surgery, can result in urethral trauma and scarring.
- Congenital Factors: Some men are born with a narrow urethra or may develop urethral strictures as a result of congenital abnormalities.
Symptoms of Urethral Stricture
The most common urethral stricture symptoms include:
- A weak or interrupted urine stream
- Painful urination (dysuria)
- Difficulty starting urination
- Frequent urination or the feeling of incomplete bladder emptying
- Blood in the urine (hematuria)
- Recurrent urinary tract infections (UTIs)
These symptoms can have a significant impact on daily life and may worsen if left untreated, increasing the risk of kidney damage and bladder dysfunction.
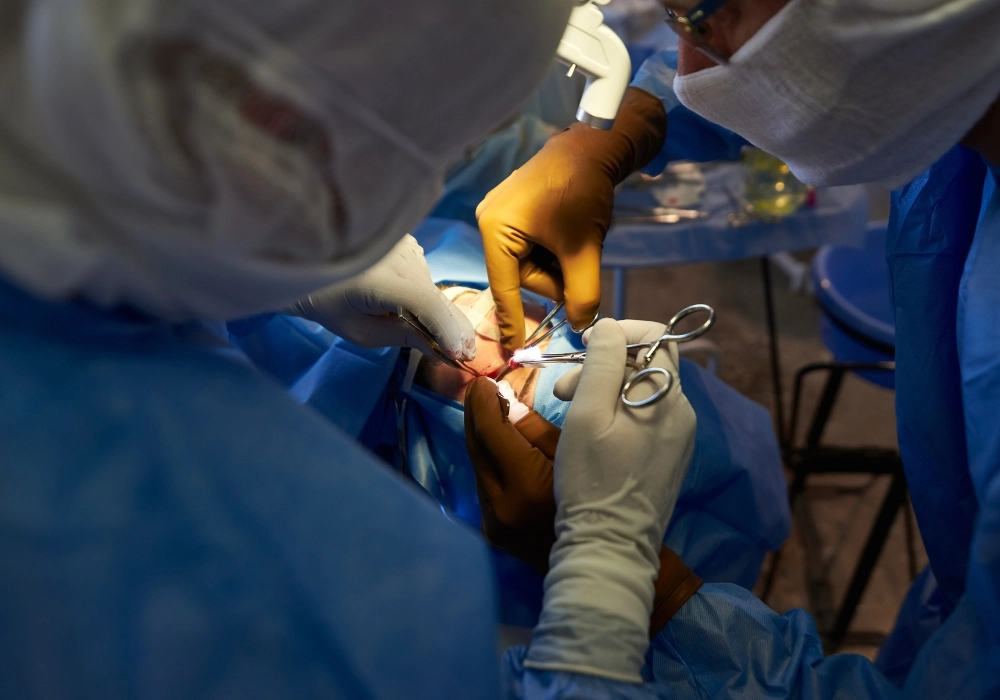
Urethral Stricture Surgery
Urethral stricture surgery is often recommended for patients experiencing significant symptoms or recurrent urinary retention due to the stricture. The goal of surgery is to remove or bypass the scar tissue and restore the normal diameter of the urethra, allowing for the free flow of urine. Various surgical techniques are available depending on the length, location, and severity of the stricture.
Several types of urethral stricture surgery are available, each designed to treat different forms of strictures. The choice of surgery depends on the severity, length, and location of the stricture, as well as the patient’s overall health and history of prior treatments.
- Urethrotomy
A urethrotomy is a minimally invasive procedure often used for shorter, less severe strictures. During this procedure, a small incision is made in the stricture using a special instrument inserted through the urethra. This opens up the narrowed area and allows for normal urine flow. While urethrotomy is effective for mild cases, there is a risk of recurrence, and follow-up treatments may be necessary.
- Urethral Dilation
This non-surgical option involves inserting a catheter or series of gradually larger tubes into the urethra to stretch the narrowed section. While effective in the short term, dilation often needs to be repeated as the stricture can return. It is typically used for less severe strictures or as an initial treatment before more invasive surgeries are considered.
- Urethroplasty
For more complex or recurrent strictures, urethroplasty is the preferred option. Urethroplasty involves removing the scar tissue and reconstructing the urethra using tissue grafts, often from the patient’s own body. This surgery offers a long-term solution and has a higher success rate than urethrotomy or dilation, especially for strictures longer than 1.5 centimeters.
- End-to-End Anastomosis
This procedure is typically used for short strictures. During this surgery, the narrowed part of the urethra is completely removed, and the healthy ends are stitched back together. End-to-end anastomosis is highly effective for shorter strictures but may not be suitable for longer or more complex cases.
Choosing the Right Surgery
The type of urethral stricture surgery recommended will depend on factors such as the length and location of the stricture, prior treatments, and overall health. Urethroplasty is considered the gold standard for longer and more severe strictures, offering the best long-term success rates. Your urologist will recommend the most appropriate treatment based on your unique condition.
Urethral stricture surgery is not always the first line of treatment for mild or asymptomatic cases. However, for patients with significant symptoms or those whose condition worsens over time, surgery becomes a necessity. Here are the primary reasons or indications for urethral stricture surgery:
- Recurrent Urinary Tract Infections (UTIs)
One of the most common consequences of untreated urethral strictures is recurrent UTIs. The blockage in the urethra can cause incomplete bladder emptying, which creates an environment for bacterial growth. If a patient experiences multiple UTIs due to a urethral stricture, surgery may be required to prevent further infections and damage to the bladder and kidneys.
- Severe or Worsening Symptoms
Patients with urethral stricture symptoms such as a weak urine stream, difficulty urinating, or painful urination often find that these symptoms worsen over time. If left untreated, the stricture can become more severe, potentially leading to complete urinary retention. Surgical intervention is indicated when symptoms significantly impact quality of life or pose a risk to kidney function.
- Urinary Retention
Urinary retention is the inability to completely or partially empty the bladder. It can occur suddenly or develop over time, leading to bladder damage, increased pressure on the kidneys, and even life-threatening conditions such as kidney failure. Urethral stricture surgery is often the only way to restore normal bladder function and prevent serious complications.
- Bladder or Kidney Damage
If a urethral stricture is left untreated for a long period, it can lead to bladder overactivity or even damage to the kidneys due to the backflow of urine (hydronephrosis). When bladder or kidney damage is detected, surgery becomes necessary to prevent further deterioration of the urinary system.
Urethral Stricture Causes
While urethral stricture causes vary, some common factors include trauma to the urethra, previous surgeries, and infections such as gonorrhea or chlamydia. In many cases, scar tissue forms as a result of these injuries or infections, leading to the development of a stricture.
Recovery following urethral stricture surgery depends on the type of surgery performed and the severity of the stricture. While each patient’s recovery process is unique, there are general guidelines and expectations for post-operative care.
- Immediate Post-Surgery Care
After surgery, patients are typically monitored in a recovery room before being discharged. If the procedure was minimally invasive, such as a urethrotomy, patients can often return home the same day. In more complex surgeries like urethroplasty, a short hospital stay may be required. A catheter is usually inserted during surgery and may remain in place for several days to help with urination and reduce strain on the urethra.
- Pain and Discomfort
Mild pain and discomfort around the surgical site are common during the first week following urethral stricture surgery. Over-the-counter pain medications or prescribed pain relievers can help manage any discomfort. Swelling in the genital area may occur but typically subsides within a few days. Ice packs and rest can help alleviate these symptoms.
- Activity Restrictions
During the first two to four weeks after surgery, patients should avoid strenuous physical activities such as heavy lifting, running, and sexual intercourse. Light walking is encouraged to promote blood flow and prevent blood clots. It’s important to follow the surgeon’s instructions carefully and attend all follow-up appointments to monitor the healing process.
- Follow-Up Care and Catheter Removal
In cases where a catheter is used, it will be removed within a week or two, depending on the healing progress. Regular follow-up appointments are essential to ensure that the urethra is healing properly and that the stricture does not recur. Urologists will often recommend imaging tests or a urethroscopy to check for any complications.
- Long-Term Care
Complete recovery from urethral stricture surgery can take a few months, particularly in complex cases involving urethroplasty. Patients should maintain a healthy diet, stay hydrated, and avoid activities that could put pressure on the healing area. Routine follow-up visits will ensure the long-term success of the surgery.
The cost of urethral stricture surgery can vary significantly depending on several factors, including the complexity of the procedure, the type of surgery, the surgeon’s expertise, and the healthcare facility. Understanding these cost factors is important for patients as they plan their treatment and recovery.
- Type of Surgery
The cost of urethral stricture surgery depends largely on the type of procedure chosen. Minimally invasive procedures like urethrotomy or dilation are generally less expensive but may require additional follow-up treatments if the stricture recurs. Urethroplasty, which involves tissue grafting and reconstruction, is more complex and may incur higher costs due to the longer surgical time and specialized care required.
- Surgeon’s Experience
A surgeon’s expertise and specialization in treating urethral strictures can impact the overall cost of the procedure. Surgeons with advanced training or those practicing in high-demand areas may charge higher fees for their services. However, selecting a highly skilled surgeon can significantly improve the chances of a successful outcome and reduce the risk of complications or recurrence.
- Hospital or Clinic Fees
Hospital fees, including anesthesia, operating room time, and post-surgery care, contribute to the overall cost of urethral stricture surgery. Outpatient clinics may offer lower costs compared to major hospitals, but the choice of facility should depend on the patient’s medical needs and the complexity of the surgery.
Insurance Coverage
Most insurance plans cover urethral stricture surgery if it is deemed medically necessary. Patients should contact their insurance provider to confirm their coverage and determine if any out-of-pocket costs, such as deductibles or co-pays, are required. It is also advisable to inquire about pre-authorization requirements to avoid delays in treatment.