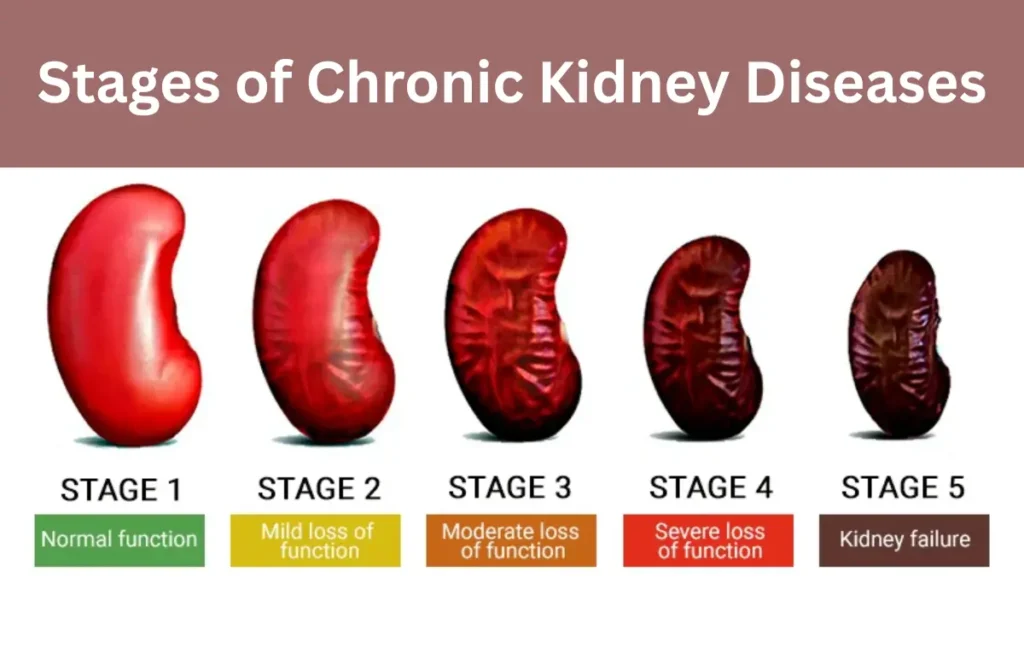
The stages of chronic kidney disease (CKD) refer to the progressive loss of kidney function over time, categorized primarily by the estimated glomerular filtration rate (eGFR). This rate estimates how well the kidneys filter waste and excess fluid from the blood. The five stages of chronic kidney disease range from mild kidney damage in Stage 1 to complete kidney failure in Stage 5. Early identification and intervention can slow or even halt the progression, minimizing complications and improving quality of life.
What do the stages of chronic kidney disease (CKD) refer to?
The stages of chronic kidney disease (CKD) describe how severely the kidneys are damaged and how well they are functioning. These stages are primarily based on the estimated glomerular filtration rate (eGFR), which is a measurement of how efficiently the kidneys are filtering waste products from the blood. The five stages of chronic kidney disease progress from normal or mildly reduced kidney function to end-stage renal disease, where the kidneys can no longer function without dialysis or a transplant.
The classification system enables medical professionals to:
- Detect early kidney damage, even when symptoms are absent.
- Tailor treatment strategies according to disease severity.
- Monitor the progression and associated health complications.
- Counsel patients on lifestyle modifications to slow kidney damage.
Each stage reflects the decreasing filtering capacity of the kidneys and increasing risk of complications, including cardiovascular disease, anemia, bone disorders, and fluid retention. Recognizing the stages of chronic kidney disease is essential for preventing severe health outcomes.
Key Features of the CKD Staging System:
- Stage 1 (eGFR ≥ 90): Normal kidney function with some evidence of kidney damage (e.g., protein in urine).
- Stage 2 (eGFR 60–89): Mildly reduced kidney function, often still asymptomatic but with signs of damage.
- Stage 3 (eGFR 30–59): Moderately reduced function; early symptoms and complications may appear.
- Stage 4 (eGFR 15–29): Severely reduced kidney function with higher risk for complications.
- Stage 5 (eGFR < 15): Kidney failure requiring dialysis or transplant; known as end-stage renal disease (ESRD).
The five stages of chronic kidney disease provide a roadmap for healthcare teams to prevent further decline and manage patient health proactively. As kidney function decreases, the impact on blood pressure regulation, waste removal, red blood cell production, and bone health becomes more pronounced.
Additional Notes:
- Staging also considers the level of albuminuria, a marker of kidney damage, which we will discuss separately.
- Early intervention is critical, especially in stage 3 CKD, where complications start to develop.
- In stage 4, the disease becomes more serious, and understanding the causes of chronic kidney disease stage 4 is vital to control progression.
Stage 1 of CKD (eGFR of 90 or greater)
Stage 1 of chronic kidney disease is the earliest phase, where kidney function is still considered normal or high, with an eGFR of 90 or greater. However, there are signs of kidney damage, such as proteinuria (protein in the urine), structural abnormalities, or a family history of kidney disease.
At this stage, many people do not experience symptoms. Despite the normal filtering rate, the presence of kidney damage indicates that the kidneys may be under stress and could worsen if left unmonitored.
Characteristics of Stage 1 CKD:
- eGFR ≥ 90 mL/min/1.73 m²
- Presence of albumin in urine, blood in urine, or imaging evidence of kidney abnormalities
- No obvious symptoms, making it important for high-risk individuals (e.g., diabetics, hypertensives) to undergo regular screenings
Key Recommendations at Stage 1:
- Lifestyle changes such as reducing salt intake, increasing physical activity, and avoiding smoking
- Control of blood pressure and blood sugar levels to prevent further kidney damage
- Regular kidney function tests to monitor eGFR and albumin levels
- Avoidance of nephrotoxic medications, like NSAIDs (non-steroidal anti-inflammatory drugs)
Understanding Stage 1 is critical because early detection allows for interventions that may halt or slow the progression through the stages of chronic kidney disease. While this stage is not life-threatening on its own, it is a warning sign—especially for those with risk factors like diabetes, hypertension, or a family history of kidney disease.
Stage 3 of CKD (eGFR between 30 and 59)
Stage 3 of chronic kidney disease is where kidney function is moderately decreased, and early symptoms or health complications may begin to appear. The eGFR falls between 30 and 59 mL/min/1.73 m², and this stage is divided into two substages:
- Stage 3a: eGFR between 45–59
- Stage 3b: eGFR between 30–44
This stage marks a turning point in the progression through the stages of chronic kidney disease, as the risk of developing secondary health issues increases.
Signs of Chronic Kidney Disease Stage 3:
- Fatigue and weakness due to mild anemia or toxin buildup
- Swelling in the hands and feet caused by fluid retention
- Changes in urination patterns, including foamy urine or increased nighttime urination
- Mild bone pain or muscle cramps as phosphate and calcium levels become unbalanced
Complications of Chronic Kidney Disease Stage 3:
- High blood pressure becomes harder to control, worsening kidney damage
- Anemia due to decreased erythropoietin production by the kidneys
- Early signs of bone disease (renal osteodystrophy) as calcium-phosphorus balance is affected
- Increased cardiovascular risk, particularly in 3b
Management Focus:
- Referral to a nephrologist for specialized care and regular monitoring
- Dietary adjustments, such as limiting sodium, potassium, and phosphorus
- Medications to control blood pressure, blood sugar, and cholesterol
- Monitoring for complications like anemia and metabolic bone disease
Understanding the signs of chronic kidney disease stage 3 and acting early can significantly slow its advancement. It is at this point that patients often begin to feel the effects of kidney dysfunction, making proactive management vital. Being vigilant here may delay the onset of stage 4, where the causes of chronic kidney disease stage 4 become more concerning and harder to reverse.
Stage 4 of CKD (eGFR between 15 and 29)
Stage 4 of chronic kidney disease indicates severely reduced kidney function, with an eGFR ranging from 15 to 29 mL/min/1.73 m². At this point, the kidneys are significantly impaired and cannot maintain balance in the body’s fluid, waste, and electrolyte levels. This stage is considered critical, as it often leads to Stage 5 (kidney failure) if not properly managed.
Understanding the causes of chronic kidney disease stage 4 is crucial, as many patients at this stage suffer from long-standing diabetes, hypertension, glomerulonephritis, or polycystic kidney disease. Identifying and treating the underlying condition is key to preventing further decline.
Symptoms Common in Stage 4:
- Persistent fatigue and drowsiness
- Swelling in the legs and ankles
- Loss of appetite, nausea, and vomiting
- Bone and joint pain
- Metallic taste in the mouth or bad breath
Causes of Chronic Kidney Disease Stage 4:
- Uncontrolled diabetes (diabetic nephropathy) damaging the filtration units
- Chronic hypertension narrowing and hardening kidney blood vessels
- Autoimmune diseases like lupus or chronic glomerulonephritis
- Genetic disorders, including polycystic kidney disease
Complications and Management:
- Severe anemia and fatigue due to decreased erythropoietin
- Electrolyte imbalance, particularly high potassium levels, which can be life-threatening
- Metabolic acidosis, a buildup of acid in the blood
- Nutritional deficiencies due to dietary restrictions and poor absorption
Medical Approach:
- Intensive monitoring by a nephrologist, including frequent eGFR and lab checks
- Preparation for renal replacement therapy, such as dialysis or transplant
- Dietary modifications to manage fluid, protein, and phosphorus levels
- Management of cardiovascular risks, as heart disease is a leading cause of death in CKD patients
Stage 4 is a warning stage in the stages of chronic kidney disease, signaling that kidneys are nearing complete failure. Proper care and early planning for Stage 5 can improve life expectancy and quality of life.
Stage 5 of CKD (eGFR less than 15)
Stage 5 of chronic kidney disease, also known as end-stage renal disease (ESRD), represents the final and most severe stage of CKD. At this point, the kidneys have lost nearly all of their function, with an eGFR of less than 15 mL/min/1.73 m². The kidneys are no longer able to filter waste, regulate fluid balance, or maintain critical electrolytes—functions essential for survival.
This stage of kidney disease demands immediate medical intervention, typically involving dialysis or a kidney transplant. Without these treatments, waste products and toxins accumulate rapidly in the body, leading to life-threatening complications.
Symptoms of Stage 5 CKD:
- Severe fatigue, weakness, and confusion
- Nausea, vomiting, and appetite loss
- Shortness of breath due to fluid buildup in the lungs
- Uncontrollable high blood pressure
- Persistent itching and restless legs
- Uremic breath (ammonia-like odor) and metallic taste in mouth
Medical Management:
- Dialysis is usually required to take over the kidneys’ filtering role.
- Hemodialysis or peritoneal dialysis may be initiated based on patient condition.
- Kidney transplant is the preferred long-term treatment for eligible patients.
- Palliative care options may be considered for those not pursuing aggressive treatment.
Emotional and Lifestyle Support:
- Nutritional counseling is essential to manage fluid, phosphorus, potassium, and sodium.
- Psychosocial support is important due to the emotional toll of dialysis or transplant preparation.
- Strict medication adherence to control blood pressure, anemia, and bone health.
Reaching Stage 5 in the five stages of chronic kidney disease signifies the urgent need for renal replacement therapy. Timely preparation during earlier stages, especially Stage 4, can ease the transition and improve outcomes.
Albuminuria Stages
While the stages of chronic kidney disease are primarily classified by eGFR, another critical factor in evaluating kidney health is albuminuria—the presence of albumin (a type of protein) in the urine. Healthy kidneys prevent albumin from leaking into the urine, so its presence often indicates kidney damage.
The albuminuria stages are graded based on the urine albumin-to-creatinine ratio (UACR), measured in milligrams of albumin per gram of creatinine (mg/g). Albuminuria is both a marker of kidney disease and an independent risk factor for cardiovascular complications.
The Three Stages of Albuminuria:
- A1 (Normal to Mildly Increased Albuminuria):
- UACR < 30 mg/g
- Considered normal; no significant kidney damage is evident.
- Common in healthy individuals and low-risk patients.
- A2 (Moderately Increased Albuminuria):
- UACR 30–300 mg/g
- Suggests early kidney damage.
- Often present in people with diabetes or hypertension.
- A3 (Severely Increased Albuminuria):
- UACR > 300 mg/g
- Indicates significant kidney injury.
- Associated with rapid progression through the stages of chronic kidney disease and higher risk for heart disease.
Importance of Albuminuria Staging:
- Refines CKD diagnosis when combined with eGFR, even if eGFR appears normal.
- Helps assess the risk of progression and complications, especially in Stage 3 and Stage 4 CKD.
- Supports decisions about aggressive blood pressure and blood sugar control.
For instance, a person with an eGFR of 65 (Stage 2) and A3 albuminuria has a much higher risk of progression than someone with the same eGFR but A1 albuminuria. Albuminuria staging complements the five stages of chronic kidney disease by identifying those who may appear stable but have underlying progressive kidney damage.
CKD Risk Factors
Understanding the risk factors for chronic kidney disease (CKD) is essential to identify individuals who are more likely to progress through the stages of chronic kidney disease. These risk factors can be modifiable, such as lifestyle choices, or non-modifiable, such as age and genetics. Recognizing them early helps in implementing preventive strategies and monitoring high-risk populations.
Primary Risk Factors:
- Diabetes Mellitus (Type 1 and 2):
- The most common cause of CKD.
- Chronic high blood sugar damages the kidney’s filtering units, increasing the risk of progressing to stage 4 and stage 5 CKD.
- Hypertension (High Blood Pressure):
- Second leading cause of CKD.
- Over time, high blood pressure narrows and weakens kidney blood vessels.
- Cardiovascular Disease:
- Heart disease and CKD often coexist and worsen each other.
- A strong predictor of rapid deterioration across the five stages of chronic kidney disease.
Secondary Risk Factors:
- Family History of Kidney Disease: Increases susceptibility due to shared genetics and lifestyle factors.
- Older Age (over 60 years): Natural decline in kidney function, making elderly more vulnerable to late-stage complications.
- Obesity: Increases the risk of both diabetes and hypertension, accelerating kidney damage.
- Autoimmune Diseases (e.g., Lupus Nephritis): Lead to chronic inflammation and scarring of kidney tissue.
- Repeated Use of NSAIDs or Nephrotoxic Medications: Can injure kidney cells, especially when used long-term or in large doses.
- Chronic Infections or Obstructions: Conditions such as recurrent urinary tract infections or kidney stones contribute to kidney scarring.
Lifestyle and Environmental Triggers:
- High-sodium diets, smoking, and lack of exercise increase the risk of CKD development and progression.
- Uncontrolled Stage 3 CKD with persistent albuminuria and hypertension increases the likelihood of developing the complications of chronic kidney disease stage 3.
Identifying and managing these risk factors is a cornerstone of public health efforts to reduce the burden of CKD and delay progression across the stages of chronic kidney disease.
Conclusion
The stages of chronic kidney disease provide a structured way to understand how kidney function declines over time, from mild damage in Stage 1 to complete failure in Stage 5. By monitoring eGFR and albuminuria, healthcare providers can assess the severity of kidney impairment and predict the risk of progression. Interventions become more critical as patients advance through the five stages of chronic kidney disease, particularly when signs such as fatigue, fluid retention, or abnormal lab values appear—especially in Stage 3, where both signs of chronic kidney disease stage 3 and early complications start to manifest.
Preventing and managing the causes of chronic kidney disease stage 4, such as long-standing diabetes and hypertension, can delay or even prevent the need for dialysis or transplant in Stage 5. Timely detection and treatment of risk factors—like high blood pressure, obesity, and nephrotoxic drug use—play a vital role in slowing progression. Recognizing the complications of chronic kidney disease stage 3, such as anemia and bone mineral imbalances, is essential to maintaining quality of life. Ultimately, a thorough understanding of the stages of chronic kidney disease, combined with ongoing monitoring and early medical intervention, offers the best strategy for preserving kidney function and preventing life-threatening outcomes.
Read also Tests to Check Your Kidney Health.




